
The groundbreaking, non-invasive metric to evaluate your lung health.
“It is frequently necessary to measure the efficiency of gas exchange in the lungs, which is often essential for many patients with pulmonary disease. Oxygen Deficit is the most informative measure of pulmonary gas exchange.”
— Dr. John B. West
Oxygen Deficit is the most informative and direct way of measuring pulmonary gas exchange efficiency. Calculated as the difference between alveolar oxygen levels in the lungs and the arterial oxygen levels in the blood, Oxygen Deficit is a precise metric of how efficiently oxygen is transported across the blood-gas barrier. 
Assessing the efficiency of gas exchange in patients is an important aspect of clinical management and is done by measuring the difference between the partial pressure of oxygen in the lung and arterial blood. The value of measuring the A-a gradient is well-established, has proven clinical utility, and has been called the most informative index of the efficiency of pulmonary gas exchange.
Oxygen Deficit can be considered a surrogate for the alveolar-arterial gradient, and it paves the way for new advancements in pulmonary medicine. Utilizing a complex algorithm, we combine the directly measured alveolar gas levels and adjust for the Bohr effect in real-time to calculate the blood oxygen level.
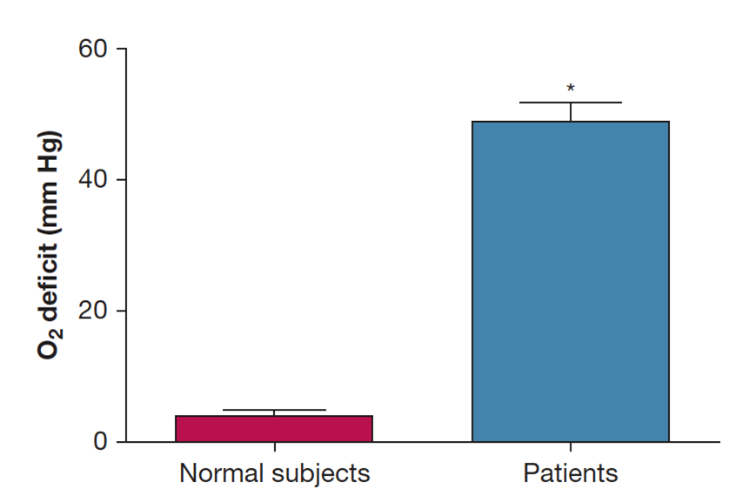
The normal range for Oxygen Deficit is 0-15 mmHg and increases with severity of disease.

The most common explanation for an increased Oxygen Deficit are ventilation-perfusion mismatches, diffusion limitations, and shunting. The normal range for Oxygen Deficit is 0-15 mmHg, depending on age. However, in patients with gas exchange abnormalities, including COPD, heart failure, pneumonia, or influenza-like diseases requiring hospitalization, Oxygen Deficit is significantly increased, with higher values indicating increasing severity of disease.
“An Oxygen Deficit of 40 mmHg or above predicted a need for supplemental oxygen at some point during that hospital course with essentially 99% accuracy. The area under the curve of the receiver operating characteristic curve was 0.99.”
Dr. Cameron McGuire - Medscape interview
Given the complexities of diagnosing and managing cardiorespiratory conditions such as pulmonary embolism, heart failure, and pneumonia, Oxygen Deficit is essential for determining the presence and extent of impairment. By identifying different causes such as ventilation-perfusion mismatches, diffusion limitations, or shunting, it helps in accurately determining the severity of gas exchange abnormalities. This enables timely and appropriate interventions, ultimately improving patient outcomes.
Oxygen Deficit has very high sensitivity to the presence of lung disease, and has been instrumental in identifying a range of cardiorespiratory complications such as pneumonia, pulmonary fibrosis, pulmonary embolism, and heart failure. Due to its sensitivity, it serves as a great patient safety measure: both in identifying impending respiratory collapse sooner and aiding in differential diagnosis. Using the MediPines AGM100, healthcare providers can accurately identify hypoxemia and quickly narrow its cause, leading to better patient outcomes and higher healthcare system efficiency.
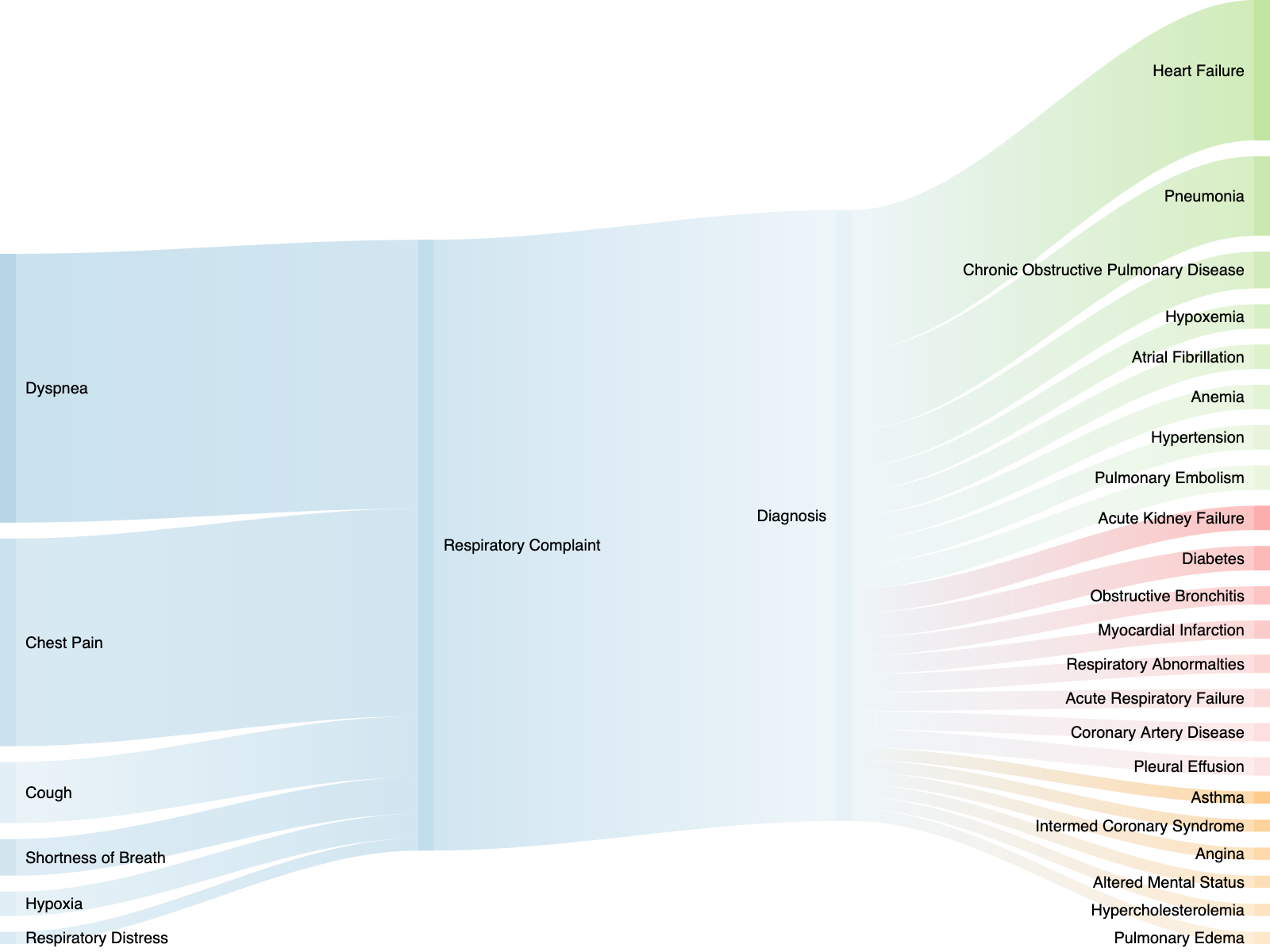
Patients in respiratory distress require immediate medical attention. The ability to quickly identify hypoxemia and its cause is crucial for positive patient outcomes. However, there is a gap in the current cardiorespiratory assessment toolkit that leaves clinicians unable to quickly identify the cause and severity of hypoxemia.
Summary
Assessing respiratory impairment precisely and accurately is critical in clinical management. The MediPines AGM100, through the non-invasive measurement of Oxygen Deficit, provides important clinical information about gas exchange efficiency at the point of care. Elevated Oxygen Deficits indicate the severity of gas exchange impairment, assisting in differential diagnosis and treatment decisions. This advancement allows for better patient care, improving outcomes and healthcare efficiency. While Oxygen Deficit provides valuable information about gas exchange efficiency, it's important to note that it should be used in conjunction with other clinical assessments and diagnostic tools for a comprehensive evaluation of cardio-respiratory conditions.
Learn more about the science behind AGM100 and Oxygen Deficit
Select Publications
Go West: translational physiology for noninvasive measurement of pulmonary gas exchange in patients with hypoxemic lung disease. Pickerodt P.A., & Kuebler W.M. American Journal of Physiology, Lung Cellular and Molecular Physiology. 2019 Mar 6;316: L701–L702. https://www.ncbi.nlm.nih.gov/pubmed/30838868
A New, Noninvasive Method of Measuring Impaired Pulmonary Gas Exchange in Lung Disease: An Outpatient Study. West J.B., Crouch D.R., Fine J.M., Makadia D., Wang D.L., Prisk G.K. CHEST. 2018;154(2), pp. 363-369. https://www.ncbi.nlm.nih.gov/pubmed/29452100
Measurements of pulmonary gas exchange efficiency using expired gas and oximetry: results in normal subjects. West, J.B., Wang, D.L., Prisk D.K. American Journal of Physiology-Lung Cellular Molecular Physiology. 2018 Apr 1;314(4): L686-L689. https://www.ncbi.nlm.nih.gov/pubmed/29351442
Noninvasive measurement of pulmonary gas exchange: comparison with data from arterial blood gases. West, J. B., Wang, D. L., Prisk, G. K., Fine, J. M., Bellinghausen, A., Light, M. P., & Crouch, D. R. American Journal of Physiology-Lung Cellular and Molecular Physiology. 2018. https://www.ncbi.nlm.nih.gov/pubmed/30335497
A lifetime of pulmonary gas exchange. West, J.B. Physiological Reports. 2018 Oct;6(20):e13903. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6198137/
Measuring the efficiency of pulmonary gas exchange using expired gas instead of arterial blood: comparing the “ideal” Po2 of Riley with end-tidal Po2. West JB, Liu MA, Stark PC, Prisk GK. American Journal of Physiology-Lung Cellular and Molecular Physiology 2020;319(2):L289-L293. https://journals.physiology.org/doi/full/10.1152/ajplung.00150.2020
Validation of a Non-invasive Assessment of Pulmonary Gas Exchange During Exercise in Hypoxia. Ainslie, Philip N., Howe, Connor A., MacLeod, David B., Wainman, Liisa, Oliver, Samuel J., CHEST. 2020 Apr. https://www.ncbi.nlm.nih.gov/pubmed/32343965