"Oxygen Deficit has high prognostic value with a fidelity that exceeds or matches the accuracy of the best predictive tools for respiratory failure in the published literature." NIH funded study, J. Clin. Med. 2025, 14, 5880
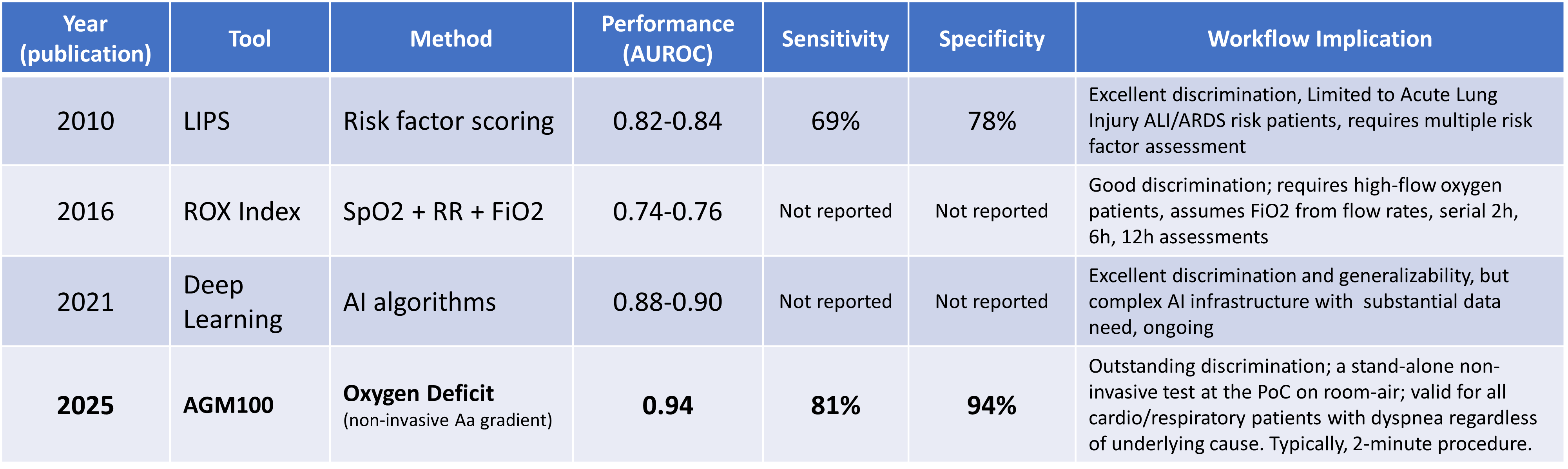
Source: NIH funded study, (J. Clin. Med. 2025, 14, 5880); discussion with comparative analysis
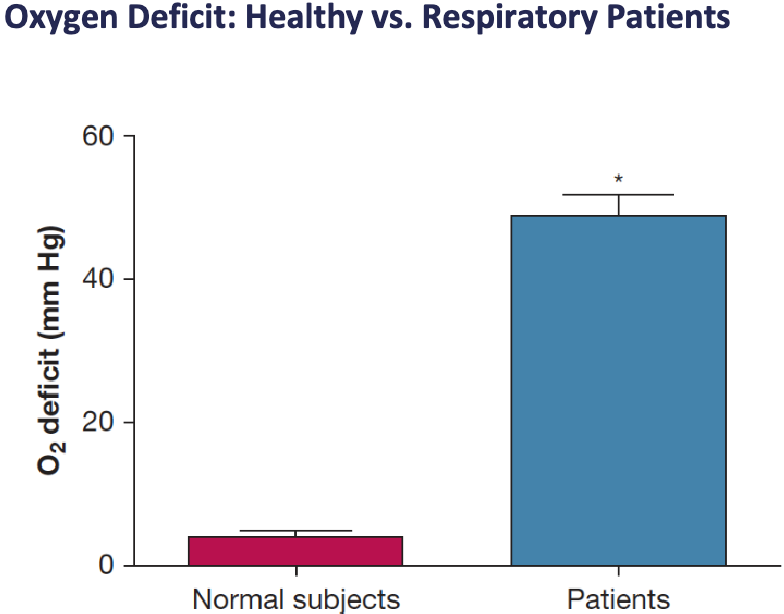
Physician-scientists evaluated how well the AGM100 could predict imminent respiratory failure in the Emergency Department, using the need for oxygen therapy within 24 hours as a real-world proxy for patient decline. The study found that across a broad range of underlying conditions, including COPD, asthma, heart failure, and pulmonary embolism, the Oxygen Deficit predicted this outcome with outstanding accuracy (AUROC 0.94) and high statistical reliability (p<0.001).
This represents the highest reported prognostic performance for any noninvasive respiratory metric. Essentially, the study confirms this tool gives clinicians an early and reliable warning sign of impending respiratory failure, allowing for more accurate triage and proactive intervention before a patient decompensates, which has major implications for improving patient safety and managing resource-intensive care.
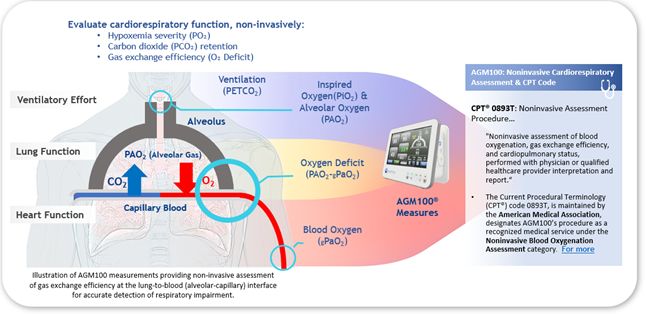
Precision in cardiorespiratory assessment is vital, and the MediPines AGM100 achieves this with comparable accuracy to Arterial Blood Gas Analysis. This near 1:1 relationship guarantees accurate and dependable measurements for better patient outcomes.
“It is frequently necessary to measure the efficiency of gas exchange in the lung, which is often essential for many patients with pulmonary disease. Oxygen Deficit is the most informative measure of pulmonary gas exchange.”
Dr. John B West
“An Oxygen Deficit of 40 mmHg or above predicted a need for supplemental oxygen at some point during that hospital course with, essentially, 99% accuracy. The area under the curve of the receiver operating characteristic curve was 0.99.”
ER Physician - Medscape interview
Pulmonary embolism (PE) is a type of venous thromboembolism (VTE) in which a clot or other obstruction breaks off and moves to the pulmonary vasculature and results in reduced pulmonary gas exchange.
There is no question that stand-alone pulse oximetry has become a standard in modern healthcare. It is as ubiquitous as the stethoscope, and as heavily relied upon as the electrocardiogram. That makes it all the more concerning that suddenly, in the midst of the largest respiratory crisis the world has ever faced, healthcare providers are wondering if this long-held lynchpin of healthcare monitoring is leading them astray.
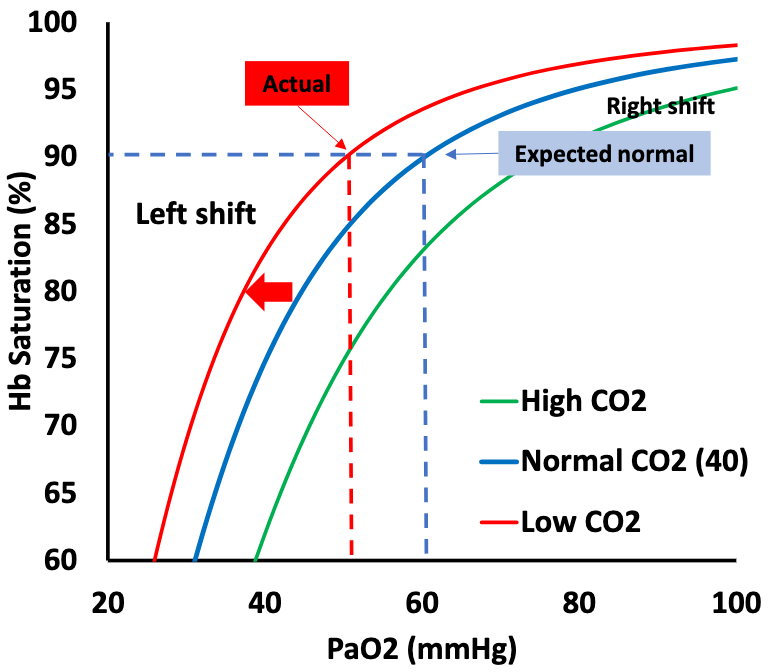
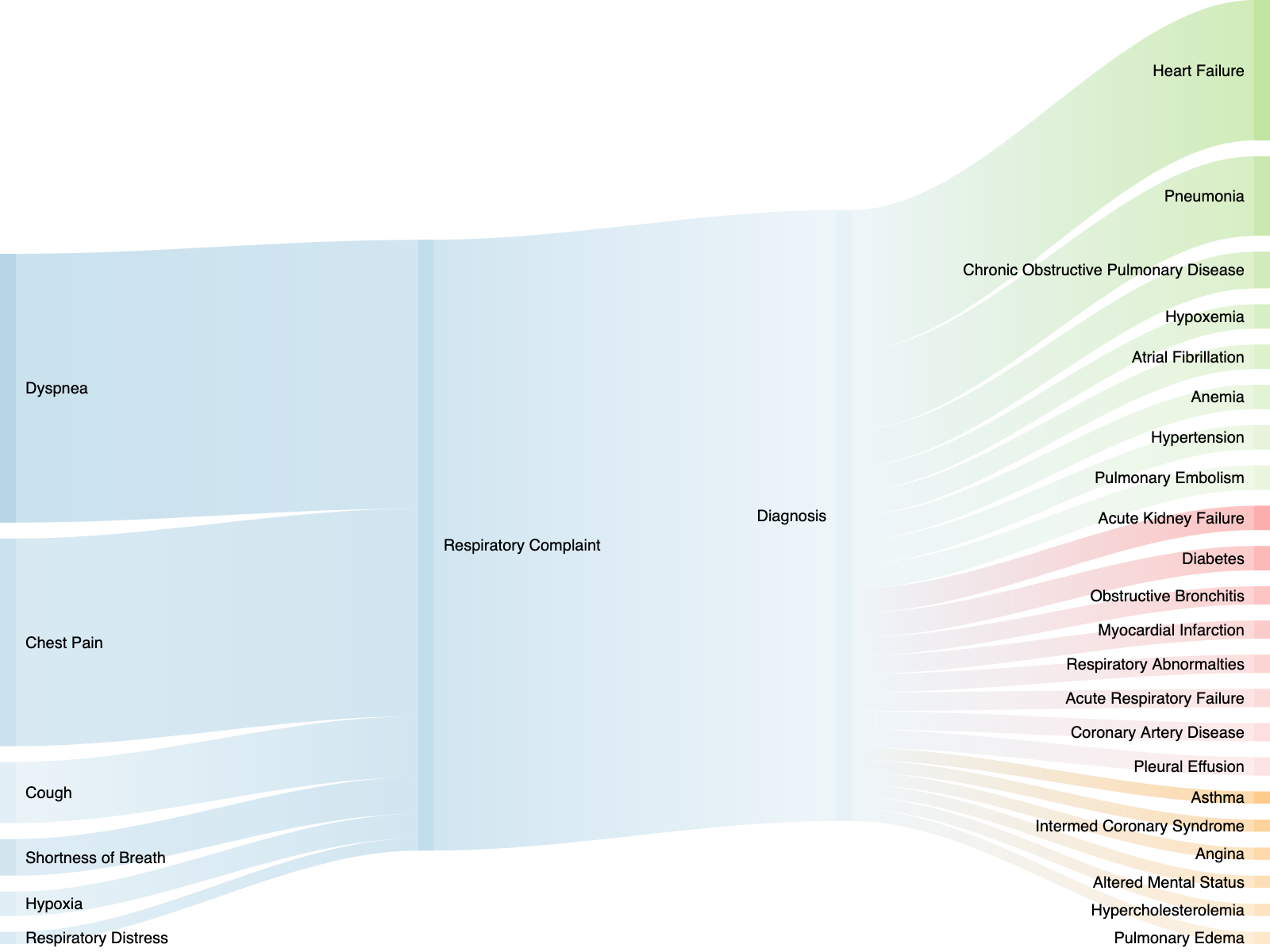
Patients in respiratory distress require immediate medical attention. The ability to quickly identify hypoxemia and its cause is crucial for positive patient outcomes. However, there is a gap in the current cardiorespiratory assessment toolkit that leaves clinicians unable to quickly identify the cause and severity of hypoxemia.
COPD patients in rural America face systemic barriers, limited access to pulmonologists, delayed diagnostics such as PFTs, and late interventions that increase the risk of hospitalization. The MediPines AGM100® bridges this gap with a non-invasive Point-of-Care solution for real-time cardiorespiratory assessment,
Go West: translational physiology for noninvasive measurement of pulmonary gas exchange in patients with hypoxemic lung disease. Pickerodt P.A., & Kuebler W.M. American Journal of Physiology, Lung Cellular and Molecular Physiology. 2019 Mar 6;316: L701–L702. https://www.ncbi.nlm.nih.gov/pubmed/30838868
A New, Noninvasive Method of Measuring Impaired Pulmonary Gas Exchange in Lung Disease: An Outpatient Study. West J.B., Crouch D.R., Fine J.M., Makadia D., Wang D.L., Prisk G.K. CHEST. 2018;154(2), pp. 363-369. https://www.ncbi.nlm.nih.gov/pubmed/29452100
Measurements of pulmonary gas exchange efficiency using expired gas and oximetry: results in normal subjects. West, J.B., Wang, D.L., Prisk D.K. American Journal of Physiology-Lung Cellular Molecular Physiology. 2018 Apr 1;314(4): L686-L689. https://www.ncbi.nlm.nih.gov/pubmed/29351442
Noninvasive measurement of pulmonary gas exchange: comparison with data from arterial blood gases. West, J. B., Wang, D. L., Prisk, G. K., Fine, J. M., Bellinghausen, A., Light, M. P., & Crouch, D. R. American Journal of Physiology-Lung Cellular and Molecular Physiology. 2018. https://www.ncbi.nlm.nih.gov/pubmed/30335497
A lifetime of pulmonary gas exchange. West, J.B. Physiological Reports. 2018 Oct;6(20):e13903. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6198137/
Measuring the efficiency of pulmonary gas exchange using expired gas instead of arterial blood: comparing the “ideal” Po2 of Riley with end-tidal Po2. West JB, Liu MA, Stark PC, Prisk GK. American Journal of Physiology-Lung Cellular and Molecular Physiology 2020;319(2):L289-L293. https://journals.physiology.org/doi/full/10.1152/ajplung.00150.2020
Validation of a Non-invasive Assessment of Pulmonary Gas Exchange During Exercise in Hypoxia. Ainslie, Philip N., Howe, Connor A., MacLeod, David B., Wainman, Liisa, Oliver, Samuel J., CHEST. 2020 Apr. https://www.ncbi.nlm.nih.gov/pubmed/32343965
John B. West, et al.
This new, noninvasive method of measuring impaired gas exchange in patients with lung disease is very sensitive to the presence of disease and may discard the need for arterial punctures in many instances.
Philip N. Ainslie, et al.
This study found that pulmonary gas exchange efficiency measured using a non-invasive gas exchange monitor provided a valid and reliable measure against directly measured arterial blood gasses at rest and during hypoxic exercise.
Download Summary
John B. West, et al.
The oxygen deficit (a surrogate for the alveolar-to-arterial oxygen difference) as calculated by the alveolar gas meter provides a useful tool for clinical triage.
This study demonstrated patients with Pulmonary Vascular Disease demonstrate a significantly elevated Oxygen Deficit and demonstrated the feasibility of testing this device in both a clinic and acute hospital setting.